Prostate cancer is the second most common cancer seen in men. Every year more than 300.0000 men around the world die because of prostate cancer. Prostate specific antigen (PSA) and digital rectal examination (DRE) are the most prevalent methods in the diagnosis of the prostate cancer. PSA is very sensitive but is not specific to prostate cancer. Just like benign prostate hyperplasia, benign pathologies can increase the levels of PSA but normal PSA levels still do not rule out prostate cancer. Prostate biopsies are evaluated histologically using the Gleason score, which is a prognostic factor of the prostate cancer and offers information about the aggressiveness level of the tumor. In addition to these findings, transrectal ultrasonography (TRUS) guided multi prostate biopsies will be used for prostate diagnosis. In some patients, after negative TRUS biopsy, clinical and pathological results indicate another biopsy.
These are as follows;
- Increasing or consistently high levels of PSA
- Suspicious DRE results
- Multiple, high levels of prostatic intraepithelial neoplasia (HGPIN ≥3)
- Presence of atypical glands adjacent to atypical, small, acinar proliferation (ASAP) HGPIN.
- Intraductal carcinoma as an isolated finding
Multiparametric MRI (Mp-MRI) is suggested for patients for whom a second biopsy is needed. Mp-MRI is important also in phasing and active monitoring in addition to its uses for prostate cancer diagnosis.
What is multi-parametric MRI (MP-MRI)?
MP-MRI does not only allow a perfect anatomic and functional screening of the prostate gland the but it also acts as a tool in the diagnosis and phasing of the prostate cancer. It also helps understand regional expansion, pelvic lymph nodes and bone metastasis in the pelvis.
Ultrasound has weak resolution which will not be sufficient for a prostate diagnosis by itself. C11- and F18- choline positron emission tomography (PET) are other imaging methods that are used to establish the reoccurrence and the presence of metastatic disease but they cannot be used for the determination of the primary tumor or the local phasing.
Who should receive multi-parametric MRI?
Patients who are suspected to have prostate cancer before biopsy (high PSA> 4.0 ng / mL and/or suspicious DRE), patients are known to have prostate cancer and for whom phasing is required (for planned curative treatment or active monitoring) and patients who are clinically suspected to have prostate cancer but whose biopsies are negative, require prostate MRG.
The place of Mp-MRI in the diagnosis of prostate cancer
In a well designed study where cancer detection rate by Mp-MRG is analyzed according to gleason score and tumer dimension for a radical prostatectomy (RP) specimen, it is observed that if the gleason score is > 7 and tumor volume is > 2 ml, the rate of cancer detection is 100%. It is known that the sensitivity of Mp-MRI in detection of cancer increases with gleason score, and index tumor status and tumor volume are the most powerful tools of tumor detection.
Prostate cancer treatment approach and multi-parametric MRI
TRUS biopsy is considered as the standard approach in primary patients. However, the fact that it is not always possible to take specimens from lesions that were targeted with TRUS and that sometimes the specimens are noncompliant with the radical prostatectomy specimens suggest that additional methods may be needed to verify the results of the TRUS biopsy. Another study showed that TRUS biopsy did not provide sufficient information about the diagnosis of the prostate cancer, the location of the tumor, about its degree or extensity. It was understood that with TRUS biopsy, it is not possible to diagnose cancers that are especially in the central lobe and in prostate apex. Today for patients whose TRUS biopsy results are negative but for which the suspicions still remain, targeted biopsy are carried out according to the results of Mp-MRI. This method became a serious alternative to saturation biopsy.
Why is multiparametric prostate MRI important?
- It is significant as it is the most sensitive prostate cancer diagnosis method and as it enables diagnosis in the earliest phase.
- These images are also important because they can be used during the prostate biopsy.
- It determines the location of the prostate tumor before the prostate biopsy and enables definitive diagnosis thanks to correct biopsy position (fusion prostate biopsy).
- It enables early diagnosis of the prostate cancer especially in males who have high PSA levels or who has a history of prostate cancer in the family.
Multiparametric MRI process and the preparation of the patient
Since hemorrhage doesn’t usually affect the visibility of the lesion in the diagnosis of the tumoral lesion, Mp-MRI can be carried out right after the biopsy. However, for local phasing purposes, a wait period of 6-8 weeks is recommended. The patient should visit the toilet before the procedure in Mp-MRI. Also, a fluid diet is recommended for the day preceding the procedure in order to prevent bowel movement artefact. It is shown that use of anti-spasmodics increased the imaging quality in more than two thirds of the patients.
How many sessions does multiparametric MRI has?
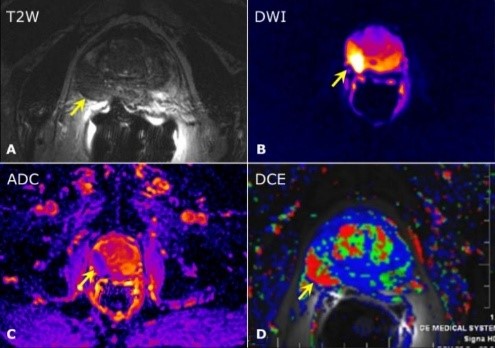
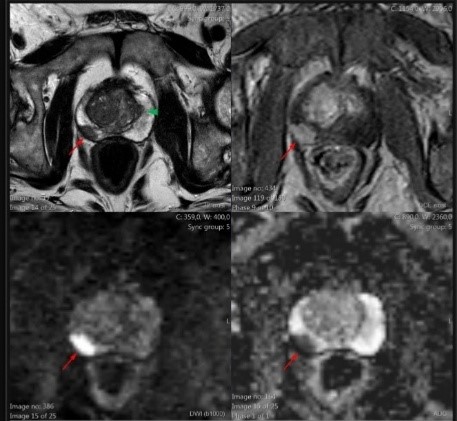
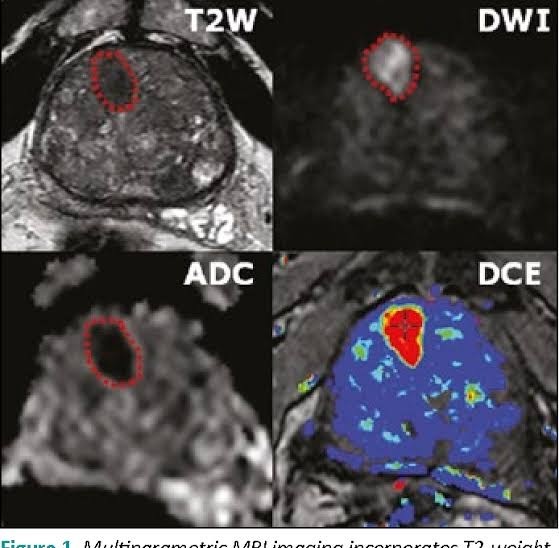
Multiparametric MRI consists of 4 sequences and is carried out in a single session.
It consists of high resolution MRI examination, diffusion-weighted MRI examination, ADC mapping and diffusion-contrast MRI examinations.
Mp-MRI sequences
Anatomic sequences
T1 weighted imaging: Since it cannot precisely determine the tumor area and zonal anatomy, it has a limited value in prostate Mp-MRI. It is not used to determine the lesion. T1A imaging helps diagnosis in biopsy-related bleeding. Hemorrhage areas seem hyperintense in T1A examination.
T2 weighted imaging: High resolution T2A examination is used for the determination of the prostate anatomy and also for the detection of the tumors. It is the most important component of MP-MRI. In T2A examination, prostate cancer in peripherical zone is usually seen with hypo-intensity. However since chronic prostatitis, calcification, atrophy, and changes after the radiotherapy can also be seen with hyperintensity it can cause misleading positive results. In such cases, according to functional sequences, the presence of the tumor is decided. T2A examination should be used with functional sequences, since it has low uniqueness in the detection of prostate cancer.
Functional sequences
Diffusion-weighted imaging:It examines the movements of the water molecules in intracellular and extracellular areas. In prostate cancer the cellular membranes prevent the permeability of the water and therefore the diffusion of the water molecules will be limited. The limitation of diffusion will be measured with b value in Mp-MRI (the quantity of diffusion weight) and apparent diffusion coefficient (ADC). It is the quantitative measurement of the ADC water molecules. In prostate cancer the b value is higher as to normal tissue; and ADC value is lower as to normal tissue.
Dynamic contrast-enhanced imaging: Provides information about the vascularization of the prostate cancer. Irregular, fragile and highly permeable neoangiogens form in prostate cancer. Before and after the application of DCE-MRI gadolinium-based contrast substance, high resolution T1A sequences are used. The contrast dynamic of the prostate cancer is very heterogenic. In DCE-MRI, the prostate cancer is contrasted earlier than normal tissue, and then reaches high concentration. The biggest problem of DCE-MRI is that it is difficult to distinguish between BPH nodules with high vascularization.
MR spectroscope: This is the imaging method that is based on the determination of some chemical metabolite in the tissues. While the choline levels increase in the prostate cancer, the citrate levels drop. The choline/citrate ratio is correlated with the Gleason score. However, since it prolongs the MRI, requires endorectal coil in 1.5 Tesla MR and a high level of experience, it is not used routinely in Mp-MRI.
Multiparametric MRI in prostate cancer scores
According to the results of multiparametric MRI, PI-RADS scoring is used for prostate cancer (prostate imaging, reporting and data system). PI-RADS v2 aims to motivate global standardization, to reduce the variation in the interpretation and reporting of the prostate Mp-MRI examinations and to improve the determination, localization and risk classification in suspicious cancer patients. However, it doesn’t deal with reoccurrence or the determination of progress during the active monitoring.

PI-RADS scoring is between 1 and 5.
- PI-RADS 1 – Very low risk
- PI-RADS 2 – Low risk
- PI-RADS 3 – Medium risk
- PI-RADS 4 – High risk
- PI-RADS 5 – Very high risk
For peripherical zone and transitional zone in PI-RADS v2, separate primary determination sequences are defined; for peripherical zone and for transitional zone, DAG and T2A sequences are accepted as primary indicative sequences, respectively. Biopsy is recommended for PI-RADS 4-5 lesions.
Biopsy decision in PI-RADS 3 lesions is still controversial. The decision must be made taking into account both clinical and laboratory results.
If cancer suspicions continue in PI-RADS 1-2 lesions, PSA generation time, PSA velocity prostate health index (PHI), urine PCA3 or 4K tests can be used to decide whether or not another ‘systematic biopsy’ is required. Since PI-RADS v2 used in Mp-MRI evaluation has subjective criteria, the sensitivity of the examination depends on the experience of the physician.
After the radiologist examines the Mp-MRI, he/she must present the report with a schematic picture and the lesion on it must be marked. This is necessary for easier determination of the location of the lesion during the cognitive biopsy and for the radiologist to be able to compare the report with the pathology results.

Can multiparametric MRI provide guidance for prostate biopsy?
Yes. Multiparametric MRI carried out when PSA is high and enables fast distinction between malignant and benign tissues. Even though PSA rises in prostate cancer, it can also increase in benign growths like Benign prostate hyperplasia. In other words, thanks to this procedure, unnecessary biopsies will no longer be a problem.
Can multiparametric prostate MRI be used even with normal PSA values?
If your specialist considers it necessary, cancer screening with this method can be used even for patients with normal PSA values.
MpMRG in active monitoring of prostate cancer
Clinically insignificant prostate cancer refers to cancer which is diagnosed through screening and which will not become symptomatic. Active monitoring is preferred when the disease does not progress and curative treatment is not required. This way, the patient is protected from the complications of the treatment. Active monitoring is suitable for the patients in selected low risk group:
- > 10 year life expectancy
- PSA ≤ 10 ng/ml
- T1c or T2a
- Gleason score ≤ 6
- Positive core count ≤ 2
- Cancer content for each positive core ≤ 50%
- PSA density < 0.15 ng/ml
Regular PSA, DRE and yearly biopsies are carried out as a part of the active monitoring protocols. Verification biopsy within 6-12 months is necessary to rule out the sampling mistakes.
Mp-MRI provides significant contributions for patient selection and patient monitoring:
- Reducing wrong classification in the beginning and in the monitoring process,
- Reducing unnecessary biopsies and facilitating patient follow-up
How is multiparametric prostate MRI is done?
It is the same as a normal MRI procedure. The patient lies down inside the MRI device and the process takes 40-45 minutes.
Will the patient be exposed to radiation in multiparametric MRI procedure?
No, there will be no radiation exposure.