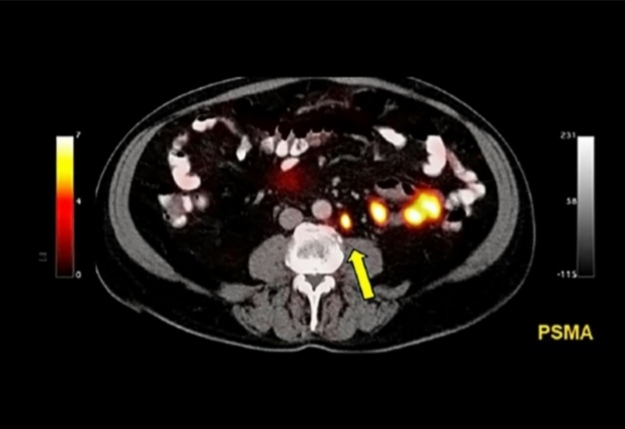
PSMA PET/BT
Surgical or radiation treatment of the cancer detected in the prostate and also at the metastasizing prostate’s surrounding tissues is described as a wasted effort. Identifying the presence/absence of metastasize immediately following the diagnosis is very important for a more optimal treatment decision for these men.
Most of the men diagnosed with prostate cancer undergo additional assays to identify an evidence for metastatic cancer. This has been performed by a conventional CT (computed tomography) scan and a bone scan for years, because prostate cancer generally metastasize to the bones.
However, both imaging technologies have limitations. Both of them are not so good to identify individual prostate cancer cells, thus very small tumors may be ignored. And bone scans may detect bone damage or abnormalities caused by an etiology other than cancer (e.g. arthritis), causing "false positive" findings that may lead to unnecessary additional assays.
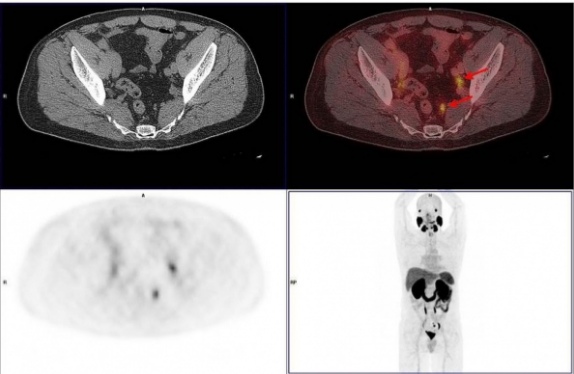
PSMA PET CT is used for patients diagnosed with prostate cancer with the suspicion of high risk for metastasis. In other words, PSMA PET -CT is also used to identify metastatic tumors in males. The ability of PSMA PET CT to detect these tumors; was higher than the standard imaging methods, such as a CT scan and a bone scan.
PSMA PET-CT has been shown to be more accurate for all far metastases including the pelvic lymph nodes and bones. The rate of radiation exposure was also lower in PSMA PET-CT.
What is PSMA-PET scan?
The scan may detect the location and extent of cancer that has recurred after initial treatment and has spread to other parts of the body. Prostate PET/CT scans may detect cancer earlier than single CT scans or MRI scans. PSMA-PET scans are the most sensitive scans to diagnose prostate tumors. So it may identify small tumors which were ignored by other scan methods. These scans may also be used by males diagnosed with a high risk or metastatic prostate cancer.
The long name of this scan is gallium-68 PSMA PET-CT. The scan has two parts - an x-ray component (CT) and a PET scan.
CT scan: CT scan uses x-rays in different directions to create a 3D image of the body.
PSMA-PET scan: PET scans use a radioactive stain to lighten specific body areas. PSMA-PET scans investigates the body areas containing PSMA protein, associated with the presence of prostate cancer cells. Gallium-68 indicates the radioactive part of the PET scan.
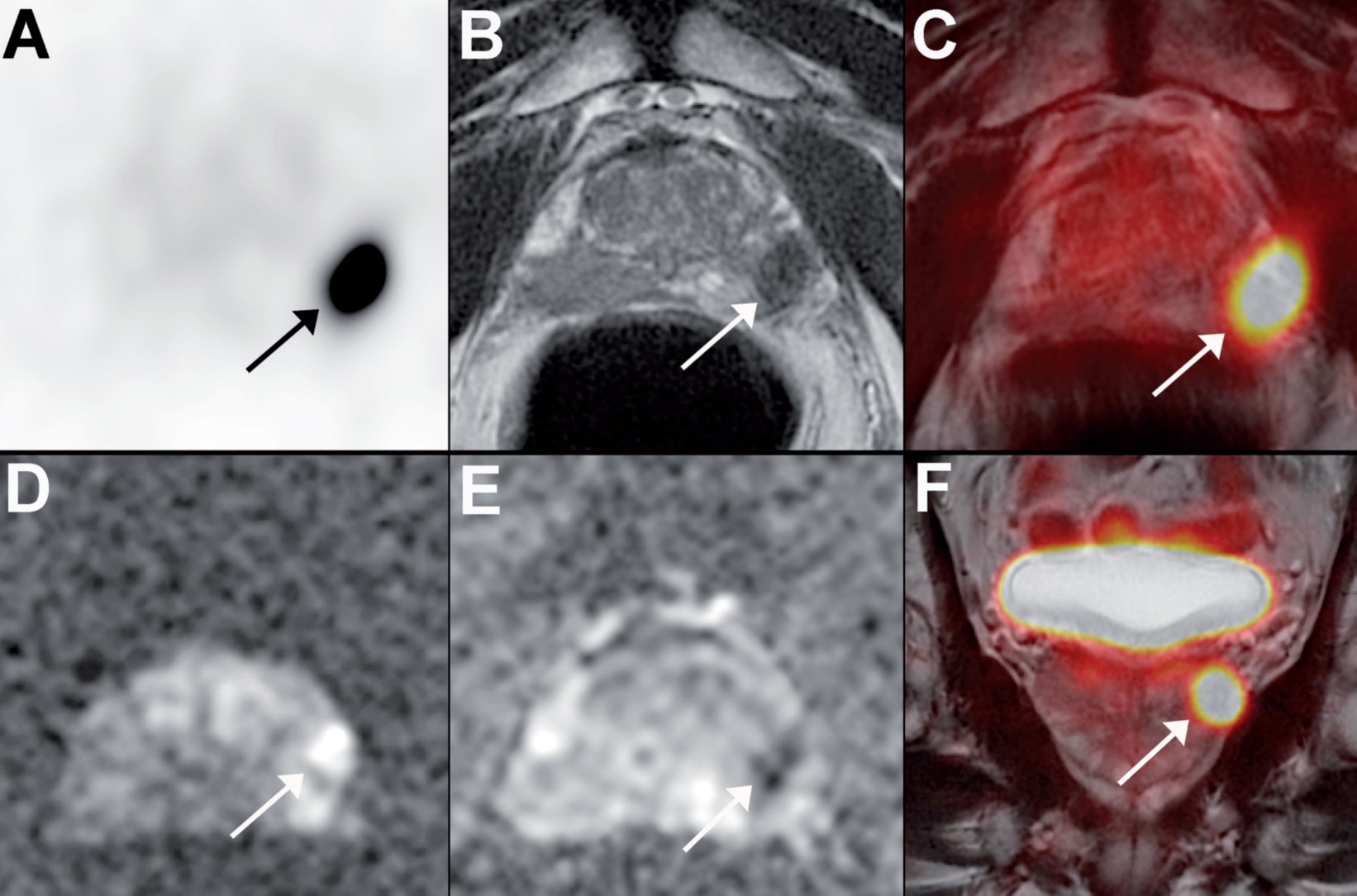
The pooled findings of CT and PET scans in a single image may show the location of prostate tumors in the body.

How does PSMA PET CT scan work?
Positron emission tomography (PET) scan is a nuclear medicine scan to monitor the intake of a small amount of liquid radioactive material in the body after the injection to the bloodstream. Many PET scans use a type of radio-labelled sugar to detect cancer because many cancers need sugar to grow rapidly. Cancers appear as "bright" in PET screening and provide additional information as compared to a standard CT scan.
What is the difference between PSMA-PET scan and a standard PET scan?
Unlike other cancers, prostate cancer usually grows slowly and generally does not appear in standard PET scans. For a PSMA-PET scan, we use a different type of radioactive tracker which specifically targets a protein called Prostate Specific Membrane Antigen or PSMA found in many prostate cancer cells. A PSMA-PET scan may see millimetric prostate cancers, so it is very good to detect the early stages of prostate cancer when it first begins to metastasize. It means that we may accurately assess the presence and the location of metastasis and adjust a better treatment for the individual conditions of patients.
Who are eligible for PSMA PET BT?
Today, PSMA-PET scans;
- are mostly used by males with increased PSA following surgery or radiotherapy treatment for localized prostate cancer. At this stage, PSMA-PET scans are the most sensitive scans to detect new tumors metastasizing despite treatment.
- individuals diagnosed with localized high-risk prostate cancer (tumors not shown by CT or bone scans).
- patients with metastatic prostate cancer at the time of diagnosis

- to determine the disease stage
- if there is a tumor suspicion, even if the biopsy results are negative,
- To clarify suspicious data in other examinations.
What are the advantages of PSMA PET CT scan?
- PSMA-PET scans are more accurate to detect or exclude metastatic tumors in men with high-risk prostate cancer at the time of diagnosis as compared to CT and bone scans
- They allow to plan more optimal treatment plans of PSMA-PET scans.
- Men who underwent PSMA-PET scans are exposed to less radiation as compared to CT and bone scans.
- Men who underwent PSMA-PET scans are less likely to get uncertain results. (The incidence of uncertain results was 23% in CT and bone scans, 7% in PSMA PET).
PSMA PET/MRI
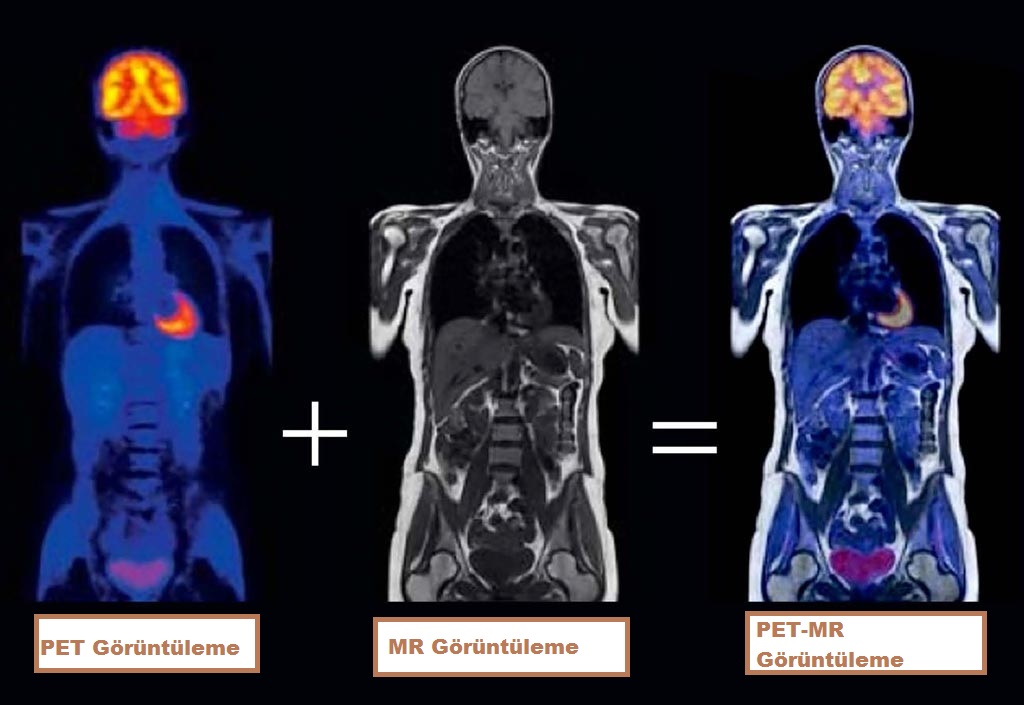
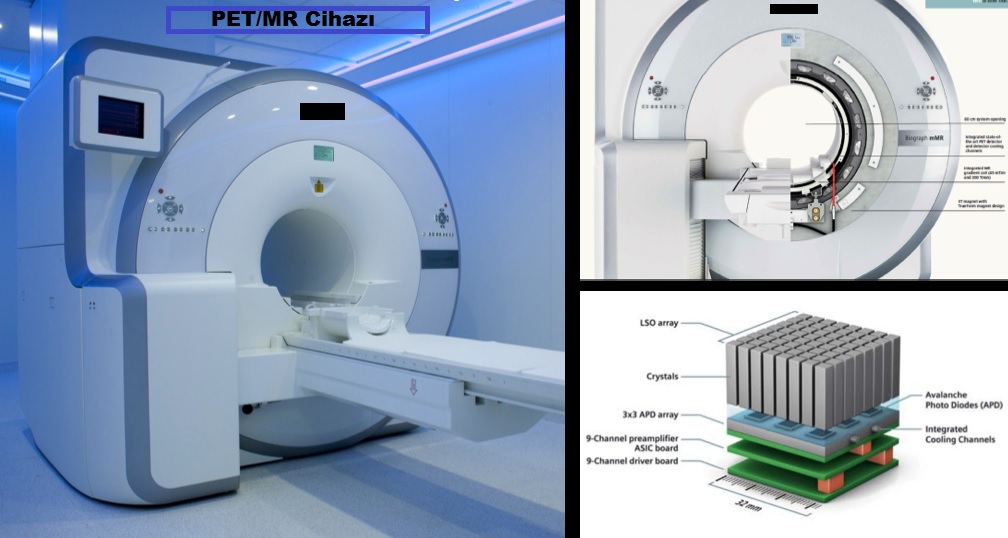
PET/MR imaging is a hybrid imaging technology that includes soft tissue morphological imaging with magnetic resonance and functional imaging with positron emission tomography.
Since PET MRI technology is formed by combining two different medical techniques, it offers advanced body scanning and imaging. With the PET MR device, which is a high-tech product, 3D evaluation can be made and the most sensitive level of information can be obtained. This screening and imaging technology is used for the diagnosis of all types of cancer.
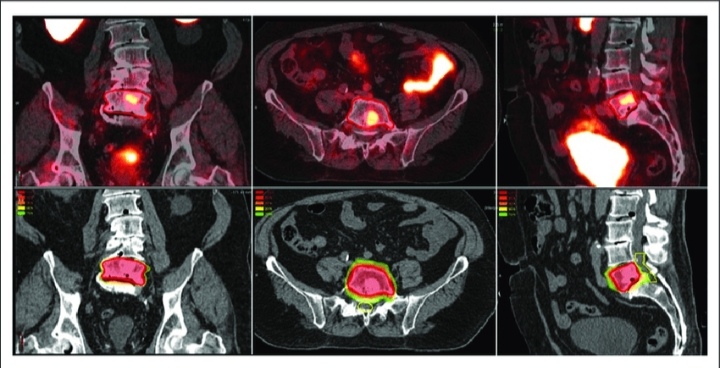
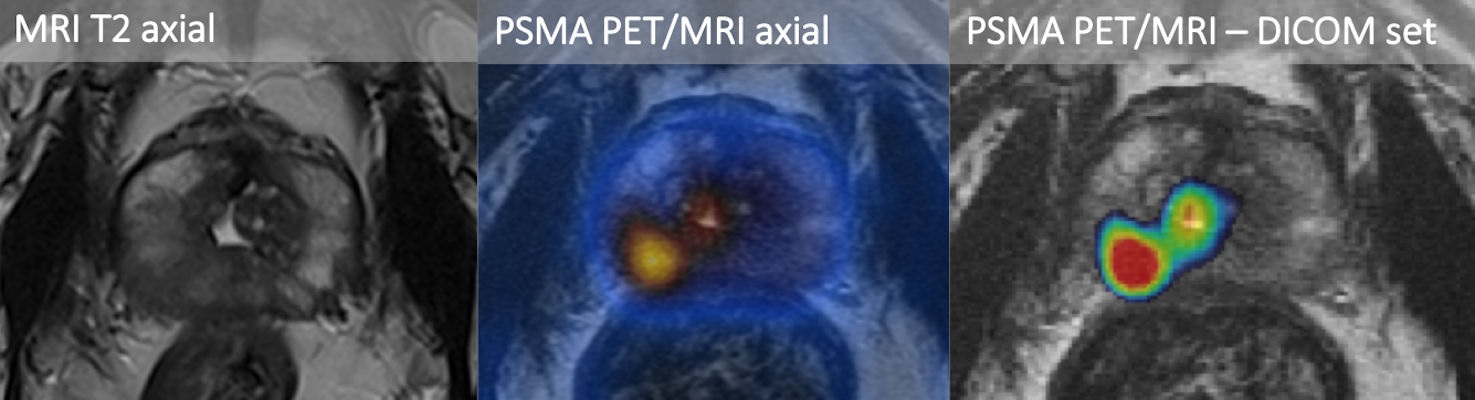
The evaluation of functional images taken with PET together with the high soft tissue contrast provided by MRI has been revolutionary, especially in tissues where CT images are insufficient in anatomical correlation, such as the prostate gland. The introduction of PET/MRI into clinical use has opened a new door for the diagnosis of prostate cancer. Prostate-specific membrane antigen (PSMA) has been extensively studied by positron emission tomography (PET), and the results have been promising. Therefore, the use of PET/MRI applications has increased in different clinical situations such as diagnosis, primary staging, biochemical recurrence detection (BCR), evaluation of therapeutic responses and treatment planning in prostate cancer imaging.
In Which Situations Is PSMA PET/MRI Preferred?
The main uses of PSMA PET MRI imaging technique are as follows:
- In cases where the inner structure of the prostate needs to be better distinguished (in the evaluation of a patient for focal therapy, PROSTATE CANCER MAP),
- Prostate cancer diagnosis and management, staging, follow-up,
- For prostate biopsy guidance and prognosis determination,
- In the differentiation of benign radiopharmaceutical involvement such as the central zone in the prostate gland and pathological involvement,
How is PSMA PET/MRI scan done?
Before undergoing PET MR scanning, there are some rules that patients must follow in order for imaging and scanning to be more successful. Patients should avoid strenuous activities and exercises 24 hours before the scan. However, he should not consume any food 6 hours before the scan. This is because blood sugar needs to be maintained at a normal level. High or low blood sugar values affect the screening results.
If you have metal or medical/mechanical devices in your body, you should inform your doctor. This examination CANNOT be performed if you have a pacemaker, defibrillator, cerebral aneurysm clip, or metal hearing aid. You must remove all your jewelry and metal objects such as hearing aids, jeans with metal zippers, piercings and removable tooth material before the procedure.
During the PET MR procedure, a radioactive substance is injected into the patient. Many patients think that this radioactive substance introduced into the body is very harmful. However, the amount of this substance given is small, it is given to the body for a short time in a way that does not cause any harmful effects. In this respect, it is less harmful than normal PET applications. Before starting the PET MR scan, the patient is injected with radioactive fluid intravenously. This process takes a very short time. The given liquid contains radioactively labeled molecules. After this fluid injection, the patient is rested for half an hour in the lead-insulated waiting room. The purpose of this waiting is to spread the radioactive fluid administered intravenously to the whole body. After waiting, the patient to be viewed and scanned is taken to the device. PET MR scanning continues for approximately 20 minutes on this device. The images obtained in detail and in high resolution are examined by the relevant experts after the completion of the process. After the examination, it is determined where the cancerous cell has spread in the body, from which point it started to spread throughout the body, and where the tumors occur in the body.
All processes take an average of 40-45 minutes. The radioactive material used in the process is quite harmless and it is ensured that scanning is carried out without being exposed to radiation. In addition, PET MR is a very useful imaging method because a better scan and image is provided with a single scan. PET MR is an imaging technique that can be widely used in children, as radiation can cause more serious effects in children.
Why Choose PSMA PET / MRI?
PET MRI combines the powers of whole-body Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) to diagnose oncologically, stage cancer cases, and evaluate treatment response. At the same time, PET MRI can be used safely in some children and young adults, which significantly reduces the risk of radiation.
PET-MR;
- Since MRI does not contain radiation, the patient receives radiation 1/3 of the PET CT examination in PET MRI.
- It offers a powerful imaging system, 3 Tesla MRI test, and a high-resolution PET scanner.
- Increases diagnostic reliability.
In conclusion, PSMA PET imaging has become an important milestone in the diagnosis and management of prostate cancer. In addition to staging, it is an important imaging method in primary lesion detection, biopsy guidance and prognosis. Especially with the introduction of PET/MRI hybrid devices, simultaneous PSMA PET/MRI imaging has the potential to change diagnosis and treatment algorithms in the future. However, it is currently used for scientific studies in clinical practice.