TRUS biopsy is considered as the standard approach in patients with prostate cancer. However, the fact that 25-39% of the prostate cancer seems isoechoic, that it is not always possible to take samples from the targeted lesions using TRUS and the noncompliance of biopsies with the radical prostatectomy specimens suggest that additional methods are needed to increase the accuracy of TRUS biopsy. Studies show that TRUS biopsy does not provide sufficient information about the diagnosis of the prostate cancer, the location of the tumor, about its degree or extensity. It was understood that with TRUS biopsy, it is not possible to diagnose cancers that are especially in the central lobe and in prostate apex. Conventional TRUS biopsy sometimes necessitates the repeat of biopsies. In the beginning, more saturated biopsies were carried out in case of the such repeated biopsy procedures. But recent years more targeted biopsies have become prevalent. Today for patients whose TRUS biopsy results are negative but for which the suspicions still remain, targeted biopsy are carried out according to the results of Mp-MRI. This method became a serious alternative to saturation biopsy.
Targeted biopsy techniques
3 different fusion biopsies were defined according to the combination of MRI images and US images;
- Cognitive fusion biopsy
- Fusion biopsy accompanied by MRI (In-Bore)
- MR-TRUS fusion biopsy

Cognitive fusion biopsy; this is done by determining suspicious areas through Mp-MRI, approximately defining this area with TRUS and then carrying out the biopsy procedure. Cognitive fusion biopsy does not require any devices other than the standard USG device. It is a practical and cheap method. However, it requires MP-MRI, USG experience and 3-D cognitive talents. In small lesions, anterior and apical lesions, targeting is difficult.

Fusion biopsy accompanied by direct MRG (In-Bore); this is the practice of taking samples for biopsy in real-time from suspicious lesions while in MRI device. The biopsy procedure on targeted lesions takes around 60 to 90 minutes. Therefore, systematic biopsy cannot be carried out during the same session with the In-Bore biopsy. In addition, costs, the difficulty of the position, the necessity of having to take MRI twice can be cited as its other disadvantages.
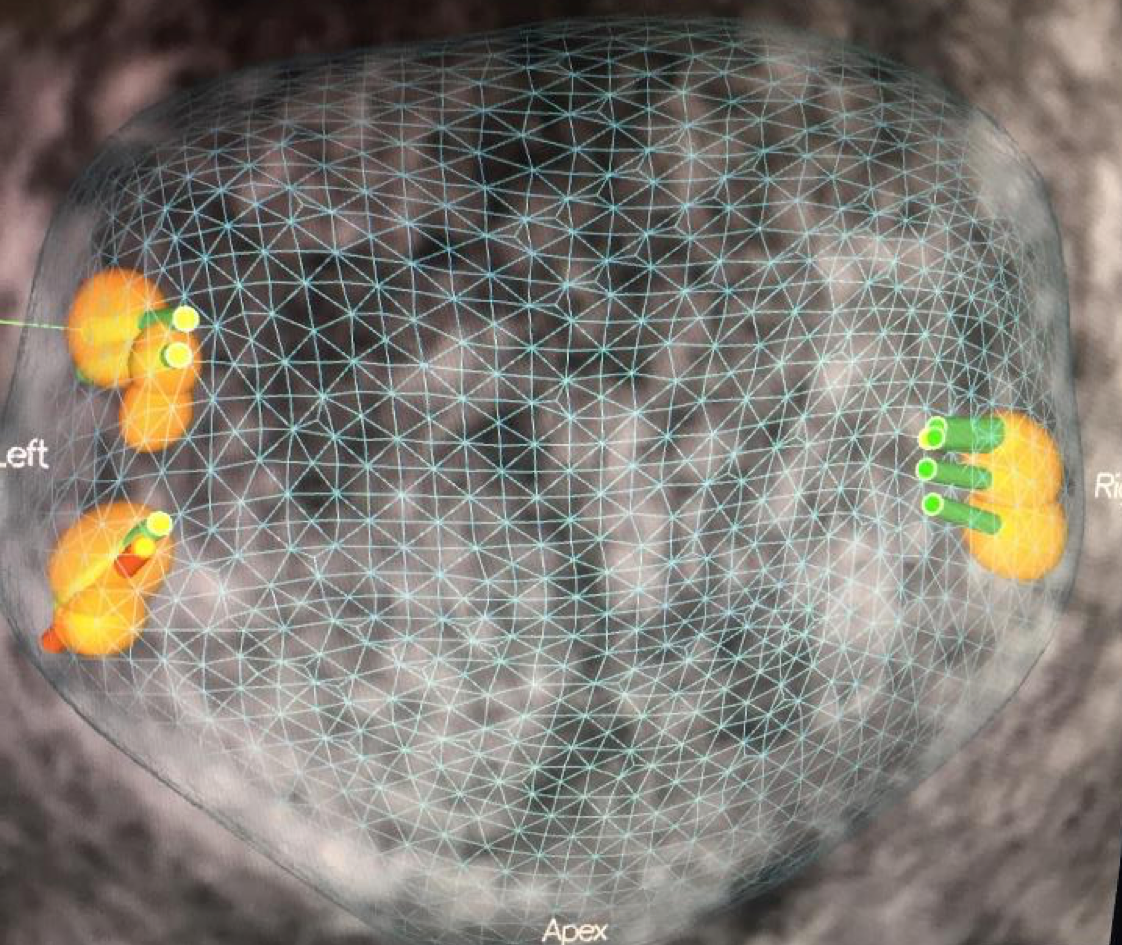
Mp-MRI/TRUS fusion biopsy; In Mp-MRI/TRUS fusion biopsy technique, MRI images are sent to a special USG-based device. The prostate will be segmented using various software and fusion will be carried out using with TRUS images. MRI and TRUS images are superimposed or placed side by side and scanned in real-time and the biopsy will be carried out on the lesion marked in MRI, with ultrasound guidance.
Advantages of Mp-MRI/TRUS fusion biopsy over cognitive fusion:
- More correct sampling depending on the lesion size
- Being able to see clearly where the sample was taken from (if the device allows that)
- More homogeneous sampling in systematic biopsy
Advantages of Mp-MRI/TRUS fusion biopsy over In-bore biopsy;
- It allows systematic biopsy in addition to sample taking from the target,
- Faster biopsy (more practical in a clinical setting)
- Higher levels of patient comfort
The length of the learning curve and the fact that segmentation procedures before the biopsy take a lot of time as well as the problems with the use of multiple devices are the disadvantages of MRI/TRUS fusion biopsy.
Prostate cancer screenings; It may include PSA blood test and DRE (digital rectum examination). If DRE or PSA tests are abnormal, the doctors can carry out TRUS biopsy with transrectal ultrasound. If the biopsy is negative the patient can be screened with regular PSA tests. However, if there is a positive DRE in the patient, or if there is a continuously increasing PSA and a negative TRUS biopsy results, prostate biopsy guided by fusion is an option for advanced screening and diagnosis.
Who should receive fusion biopsy?
If despite negative prostate biopsy results, the prostate cancer suspicions continue for a patient, MRI fusion biopsy should be carried out. Because according to the researches, one in every four people with negative biopsy results, develops prostate cancer within the next 20 years. This is also suggested for patients who have abnormality in digital rectum examination or who has high PSA values.
How is fusion biopsy done?
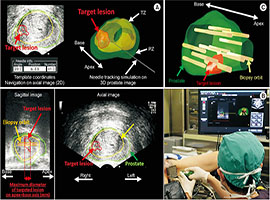
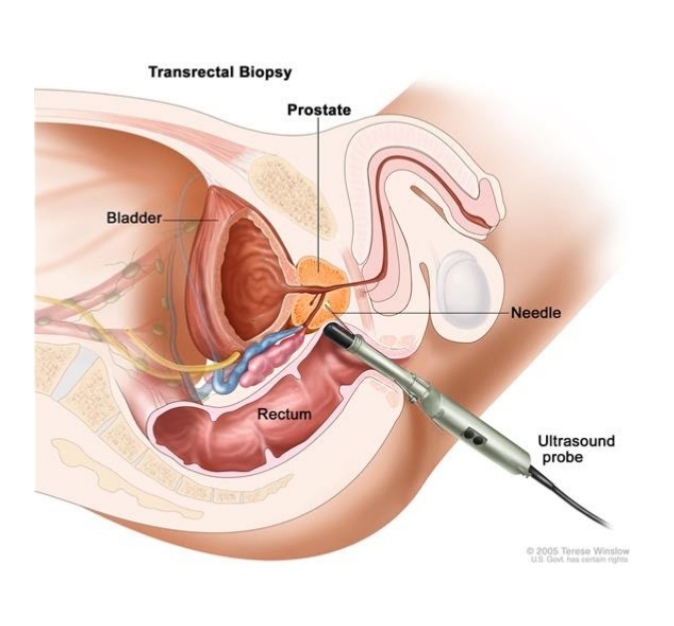
Multi-parametric MRI of the prostate will be done for pre-biopsy patients. The images on the MRI will be used to determine the suspicious areas for cancer and those areas will be marked on the images. In the meantime, the patient will be sedated and an ultrasound probe will be placed inside the rectum of the patient and the prostate will be imaged. 3D multi-parametric MRI images of the prostate will be superimposed on the ultrasound images from the rectum probe. This is why it is called fusion biopsy. Then the biopsy needle will be taken to the marked area and the sample taking process will be completed.
Number of samples to be taken from the suspicious lesion with the Mp-MRI/TRUS fusion biopsy
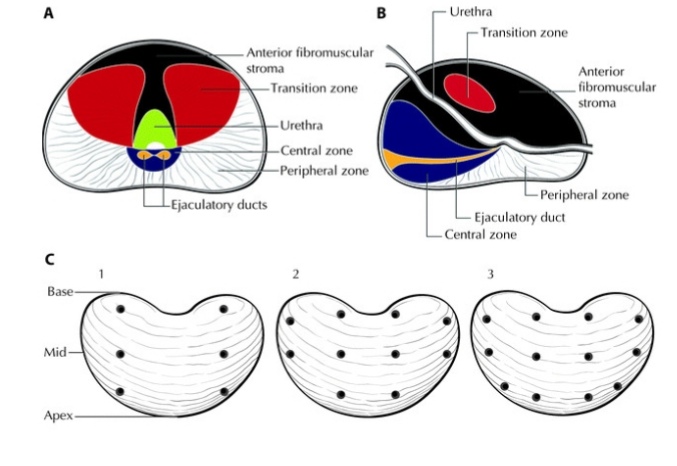 Both EAU and AUA prostate cancer guides do not provide an exact suggestion as to the number of samples that should be taken from the lesions determined through Mp-MRI. Studies show that this number can change but it is important to take at least two samples from the suspicious lesion.
Both EAU and AUA prostate cancer guides do not provide an exact suggestion as to the number of samples that should be taken from the lesions determined through Mp-MRI. Studies show that this number can change but it is important to take at least two samples from the suspicious lesion.
What are the advantages of fusion biopsy over conventional prostate biopsy?
- Fusion method creates a three-dimensional map of the prostate and directs the biopsy needle to the areas that are suspected to be cancerous.
- In patients that receive conventional biopsy treatment, aggressively spreading prostate cancers can be overlooked but fusion biopsy is more likely to catch them.
- In the conventional biopsy, depending on the number of those tissues that are taken, the risk of infection and septic complication are high despite the preventive measures. This fusion biopsy is done only on the target, therefore the number of samples will be lower, which reduces the risk of infective complications.
In summary, it is useful because;
- It will accurately determine the suspicious areas which need additional examination
- It can reduce the number of tissue samples that are needed
- Less painful and lower risk of infection and bleeding

What preparations are required before the biopsy?
Before the procedure, antibiotics will be administered for a couple of days in order to reduce the risk of infection. The patient should not use blood thinning medications like aspirin. If the patient has been using such medication, it is important that the patient stops taking that medication for one week under the supervision of a doctor. It is important that the patient stops eating within the last six hours before the procedure. Since the rectum must be empty during the procedure, patients who suffer from constipation might need to use laxatives.
How long does the procedure take?
The procedure takes 15 to 25 minutes.
Will the procedure be painful?
Thanks to anesthetic medication patients usually do not feel any pain during fusion biopsy.
What is the post-biopsy procedure?
For one week after the biopsy, there can be blood in the urine, feces and the semen for three months. This is no reason to worry and bleeding will stop by itself. The latest EAU guide suggests use of oral or intravenous antibiotic use before the biopsy and recommends the quinolone antibiotics as the first choice. However, the resistance of local antibiotics should also be taken into account. If fever is encountered during this time (it is rarely observed), a doctor should be consulted.
What should the patient do after the biopsy?
The patient must drink plenty of water and eat fiber-rich food after the procedure to avoid constipation.
Is transrectal method the only way to carry out fusion biopsy of prostate?
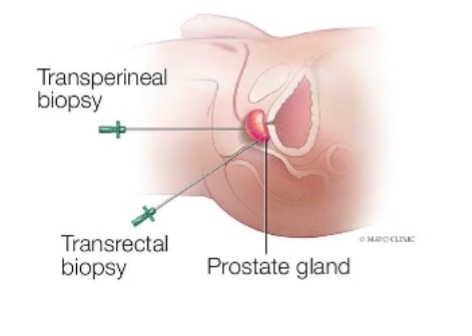
In suitable patients, the biopsy can be carried out transperineally (the area between the testicles and the rectum) instead of transrectal area. This further lowers the infection risk levels.
- Placing the needing through the rectum wall (transrectal biopsy). This is the most common method of prostate biopsy.
- Placing the needle through the skin between the rectum and the scrotum transperineal biopsy). A small incision will be cut in the skin between the rectum and scrotum and the biopsy needle will be placed inside the incision and towards the inside of the prostate to remove a tissue sample. MRI screening will guide the process.
What are the possible side effects of the biopsy?
Hematuria (blood in the urine) is the most common complication after the prostate biopsy (20-63%), and usually completely goes away after a couple of days.
Hematochezia (blood in the rectum) is also common and is seen in 2-22% of the patients. Hematospermy (blood in the ejaculation) is a clinically insignificant problem and is seen in 50% of the patients after the procedure and can continue for a couple of months. Most of the contagious complications are easily treated with antibiotics. However, there are reports of fatal sepsis cases after prostate biopsy.
Our page is for informational purposes. Consult your doctor for Diagnosis and Treatment.