In our country and world, prostate cancer is the second most common cancer in males after lung cancer. A lifetime risk of prostate cancer is one of 6 men.
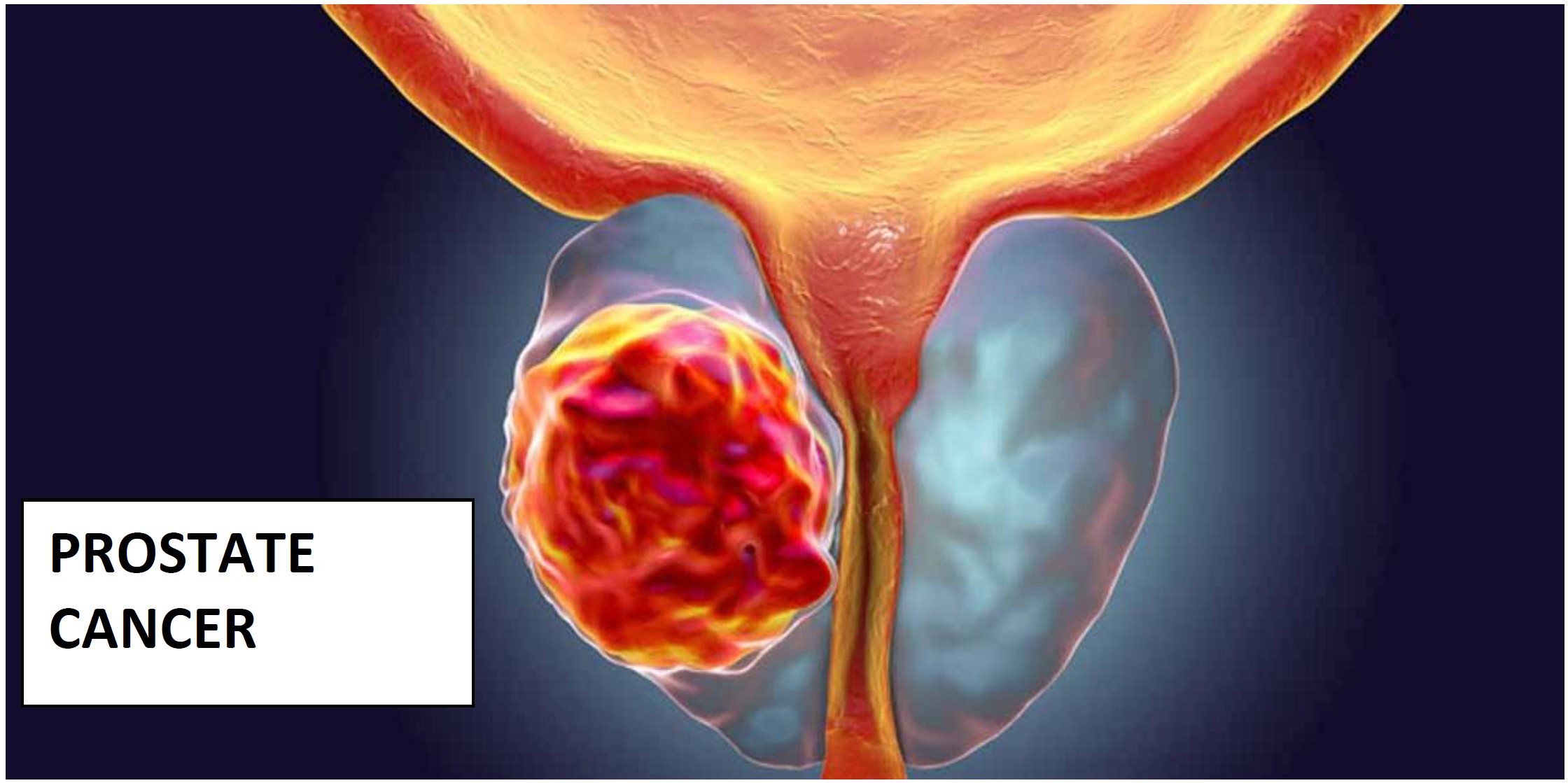
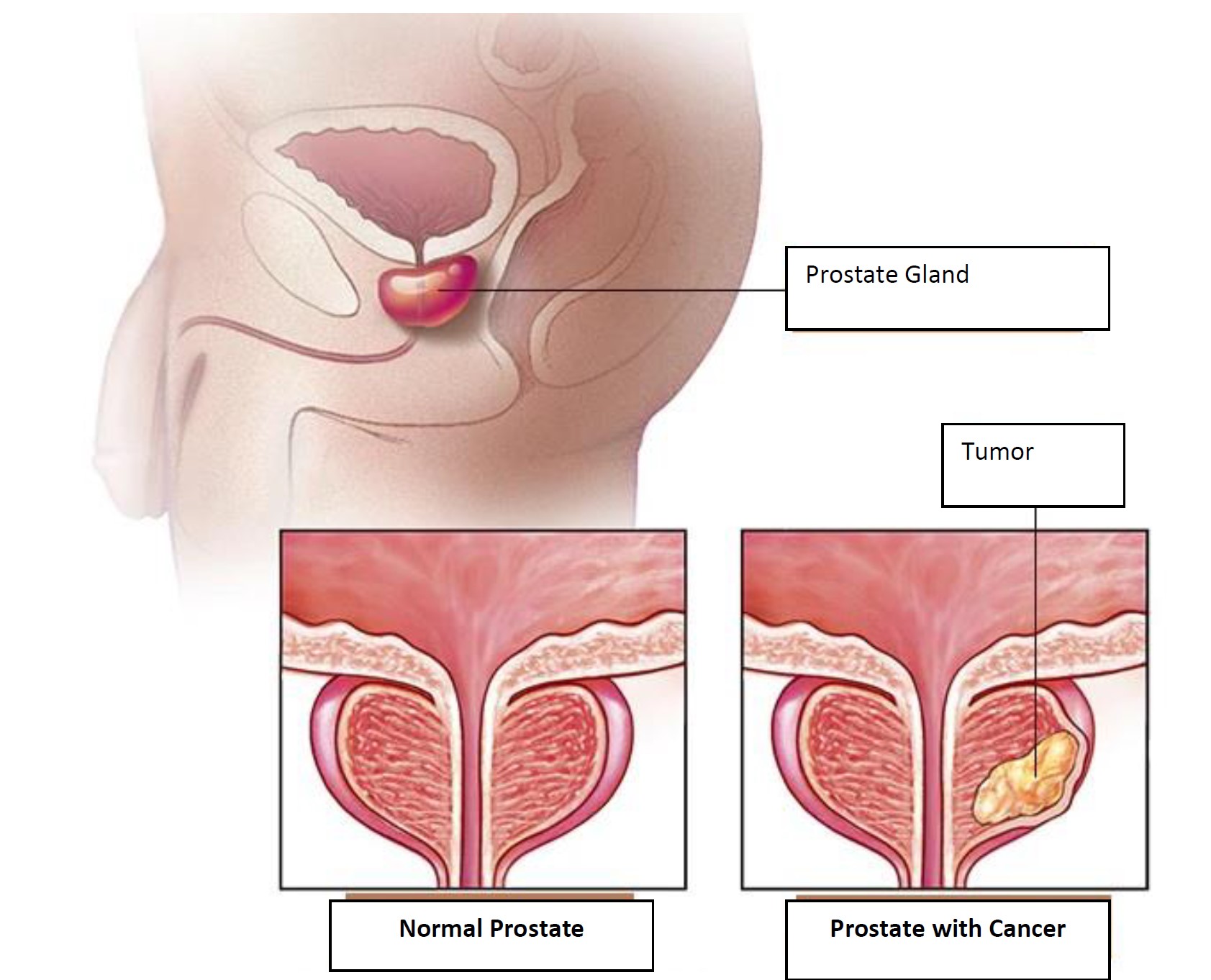
The prostate is a gland that is belong to male reproductive system. It is located under the bladder (urinary bladder). Prostate cancer may develop as a result of uncontrolled proliferation of the prostate cells. The uncontrolled cell proliferation leading to prostate cancer firstly spreads within the prostate and then may spread from the capsule around the prostate to the surrounding tissues.
Prostate cancer generally develops slowly and may be initially limited to the prostate gland without any severe damage. However, several types of prostate cancer grow slowly and require a little or no treatment, while other types are aggressive and may spread rapidly.
Etiology of Prostate Cancer
The etiology of prostate cancer is not clearly understood. Prostate cancer may develop due to both genetic and non-genetic factors. Genetic factors are inherited and cannot be changed. However, environmental factors such as lifestyle choices including diet, exercise, smoking and alcohol use are non-genetic factors and it is possible to change them.
Doctors may diagnose prostate cancer when the cancer differentiates several abnormal cells in your prostate. Mutations in the DNA of abnormal cells increase the rate of cellular proliferation and these cells are divided faster than normal cells. Abnormal cells continue to live while other cells die. The accumulated abnormal cells become a tumor that may spread to invade neighbor tissue. Several abnormal cells may also break down and spread (metastasize) to other parts of the body.
The primary factors that may increase your risk of prostate cancer include:
- Age. Your risk of prostate cancer increases with age.
- Race. Due to the unknown reasons, the risk of prostate cancer in black men is higher than other races. The risk of aggression or progression of prostate cancer is higher in black men.
- Family history. Your risk may be increased if males in your family have prostate cancer. Besides, if you have a familial gene history (BRCA1 or BRCA2) which increases the risk of breast cancer or a very strong breast cancer history, your risk of prostate cancer may be higher.
- Obesity. Obese men diagnosed with prostate cancer may be more likely to have a disease progression which is more difficult to treat.
Symptoms of Prostate Cancer
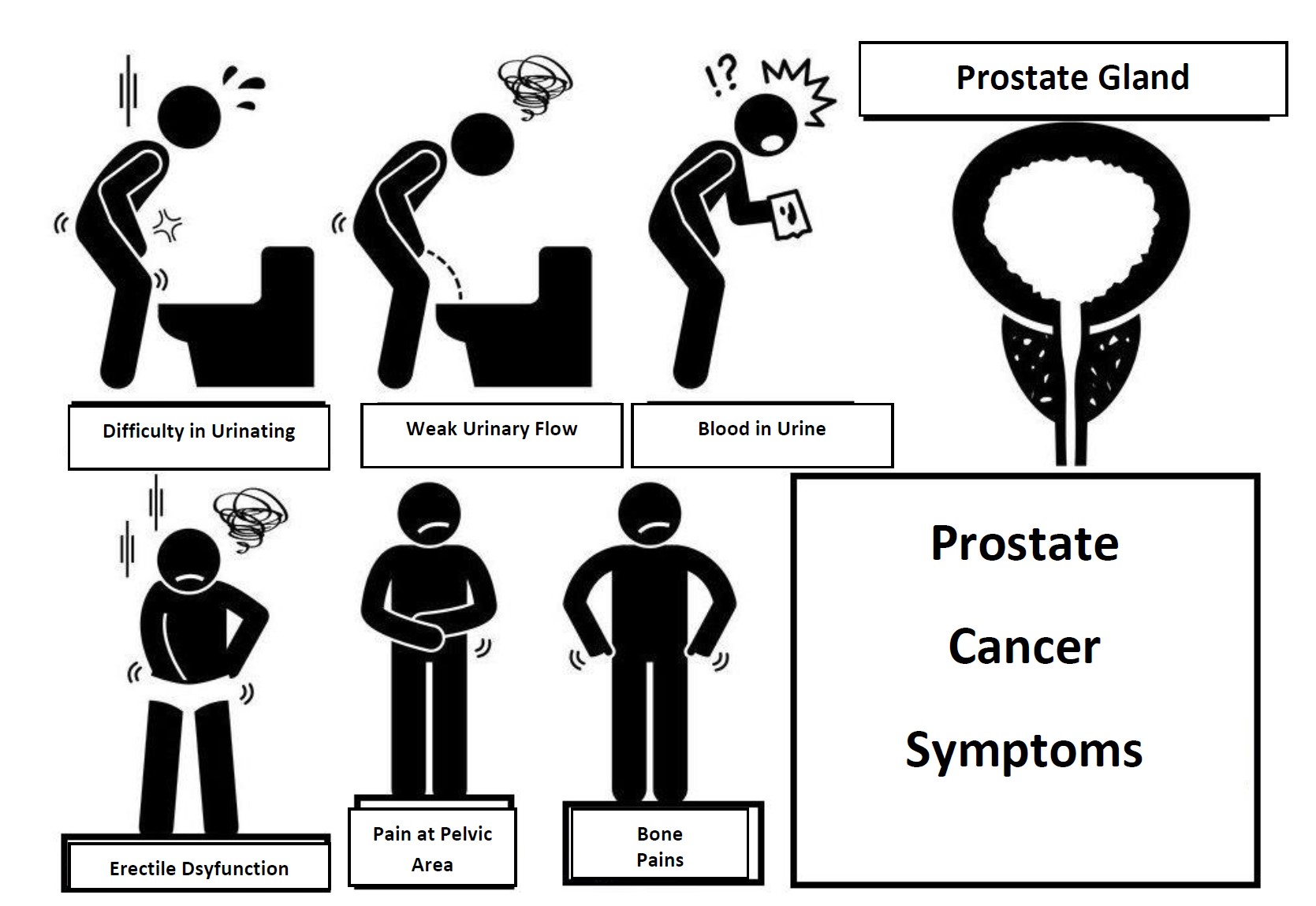
Early stage prostate cancer may cause no signs or symptoms.
A progressed prostate cancer may cause the following signs and symptoms:
- Urination problem, oliguria, urinary frequency especially in the evening,
- Decreased urinary output
- Blood in urine
- Pelvic discomfort
- Bone pain, pain in the hip, back (spine), chest or other parts of the body due to the bone metastasis,
- Erectile dysfunction (medical term: impotence)
The same symptoms may occur in other diseases. For example; difficult urination may be a symptom of benign prostatic hyperplasia (BPH) rather than cancer. Nevertheless, when such symptoms occur, you should visit an expert doctor immediately for the required early diagnosis and rapid treatment initiation.
Screening and Diagnosis in Prostate Cancer
Screening in prostate cancer is a complicated and controversial issue. There is no sufficient evidence showing that screening tests could reduce the vital risk factor in prostate cancer. Besides, all screening tests pose some risks. One of the risks in screening tests for prostate cancer is overdiagnosis (diagnosing a painless cancer causing no problems during the lifetime of a man). Overdiagnosis may lead to unnecessary cancer treatment. In other words, since the prostate cancers in our body has a slow course, they may be detected even if they would not harm us, but treatments to be applied for them with the harm potential raises questions about the screenings due to the nature of prostate cancer.
Screening tests in prostate cancer are as follows;
- A blood test measuring the level of protein known as prostate specific antigen (PSA)
- Digital-rectal examination (DRE)
- Biopsy and/or
- Transrectal ultrasound.
PSA blood test in prostate cancer diagnosis: PSA is a protein produced by cells normally found in the prostate, and is determined by a simple blood test. The PSA level determined in a patient diagnosed with prostate cancer roughly reflects the total amount of cancer. A high PSA level may indicate the presence of prostate cancer cells or other noncancerous forms of prostate. In addition, the PSA level is very helpful to follow up the success of the treatment or to determine the recovery after surgery.
Digital rectal examination (DRE): Digital rectal examination is performed with a finger using an oily glove. The prostate is touched and abnormalities are examined by their size and features. This method has been used as a standard prostate screening test for years. Normally, the prostate tissue is slightly felt in the rectal wall during digital rectal exam. Its surface is not rough and its consistence is soft. If it is hard and an irregularity was felt on the surface during digital rectal exam, these are considered as important examination findings for prostate cancer.
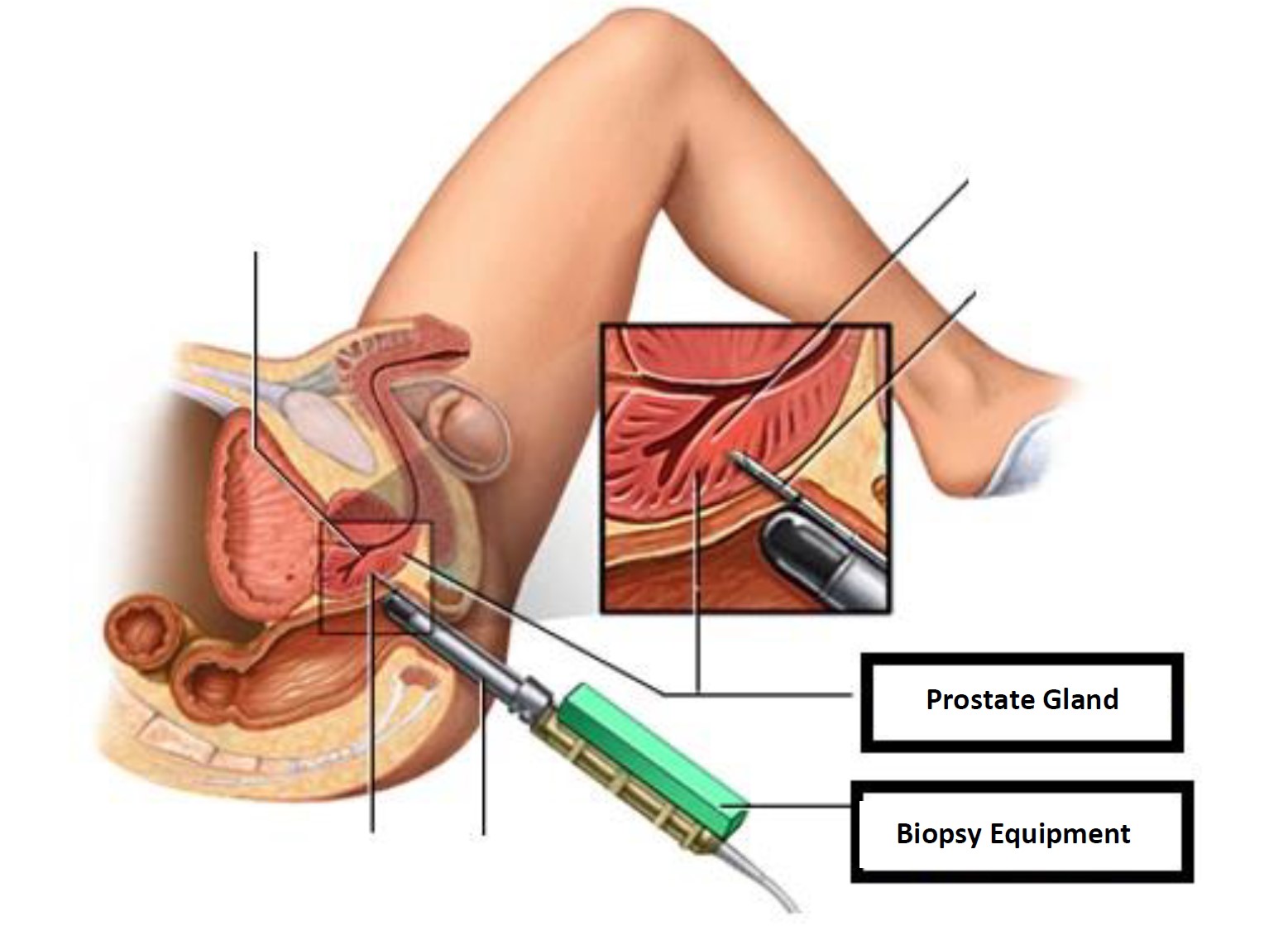
Prostate biopsy is a procedure to remove suspicious tissue samples from the prostate. If the results of the first tests, including prostate specific antigen (PSA) blood test or digital rectal exam, indicate that you may have prostate cancer, your urologist may recommend a prostate biopsy. The prostate is a small, walnut-shaped gland producing fluid to nourish and carry sperm in males. During a prostate biopsy, a needle is used to take tissue samples from your prostate gland. The procedure is performed by a doctor specialized in the urinary system and male sexual organs (urologist).
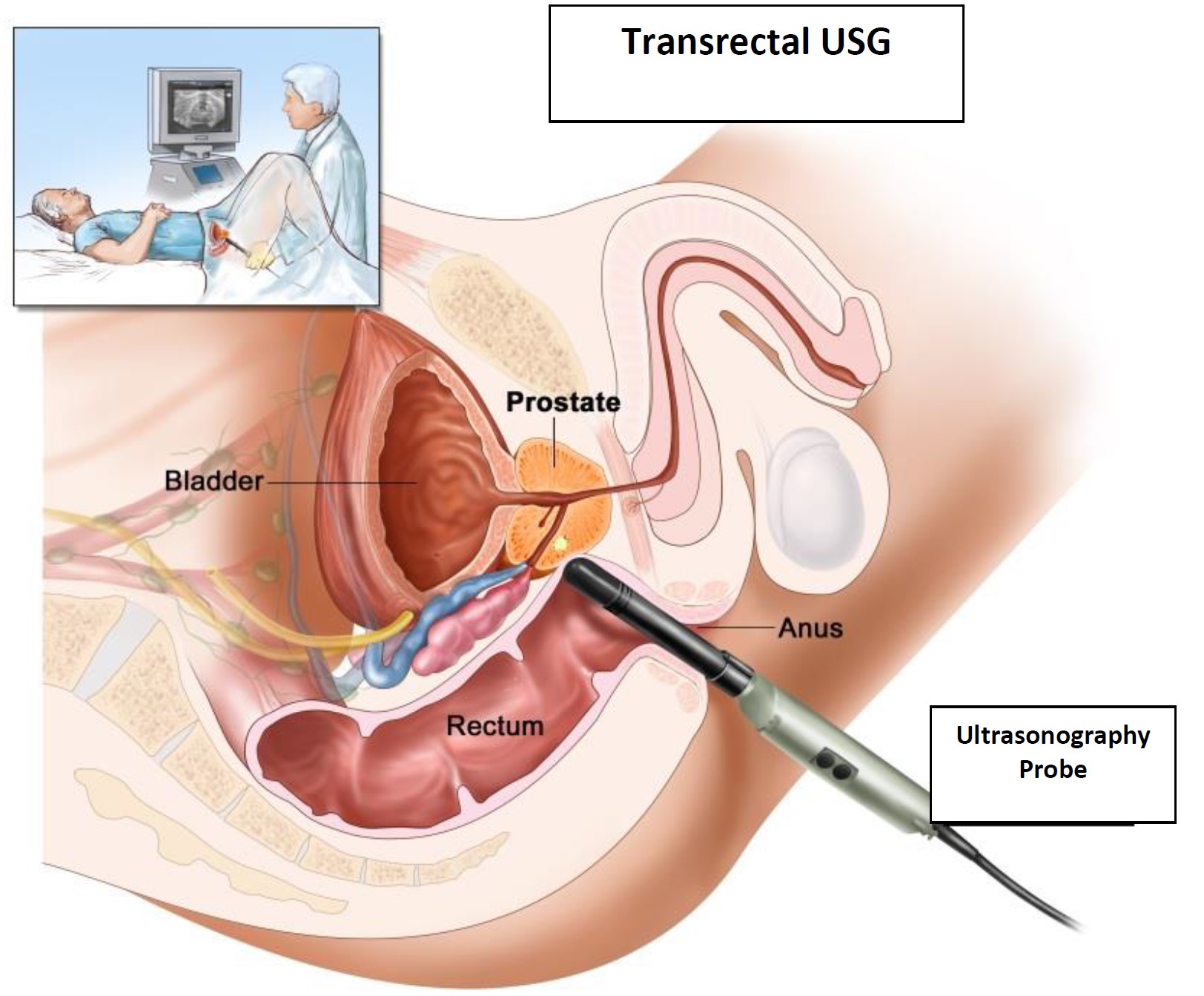
Transrectal ultrasonography in the diagnosis of prostate cancer: During transrectal ultrasonography, a small probe is inserted through the rectum. The probe emits high frequency sound waves generating echo and they return after hitting the prostate. The computer generates a picture by the sonogram showing abnormal areas using these echoes. The data showing that the transrectal ultrasonography reduces the vital risk in prostate cancer by early diagnosis are investigated.
New Procedures
What are New Diagnostic Methods?
MR has been developed. Several features are added to classical MR images, "Multiparametric Prostate MR" method has been introduced in the urology. For patients with a prostate cancer suspicion, firstly, we perform a "Multiparametric Prostate MRI" in an experienced radiology center. This MR marks the high-risk cancer areas in the prostate and transfers the images to a CD.
We plan a biopsy for our patient and match this CD with the ultrasound images by a computer during biopsy, and thus we may see the biopsy areas in 3-dimensional ultrasound like an MR image.
Thus, we take samples indicated by MRI under the guidance of MRI, not from random areas of the prostate. In other words, this biopsy is performed by MRI and ultrasound combination, called as "Fusion biopsy", fusion literally means "combination, combined", meaning that the urologist performing biopsy by Multiparametric Prostate MRI will transfer the MR images to the ultrasound and takes the samples from the marked areas. In other words, the combination of ultrasound with Multiparametric Prostate MR + Biopsy ...
MR-Ultrasound Fusion Biopsy: "smart” biopsy robot and advanced computer software allow MR images to be seen in ultrasound and to take samples from the correct target areas.
Staging Prostate Cancer
A subject diagnosed with prostate cancer undergoes blood tests, blood PSA level, chest radiography, upper abdominal ultrasound, MRI of the lower abdomen and prostate to identify the spread (stage) of the disease.
Following needle biopsy, classification is made by Gleason Score System (Gleason Score). This classification is evaluated on a 2 to 10 scale. This scale gives information about the aggression of the cancer. A higher Gleason score indicates a more aggressive cancer with the potential of faster proliferation and metastasis.
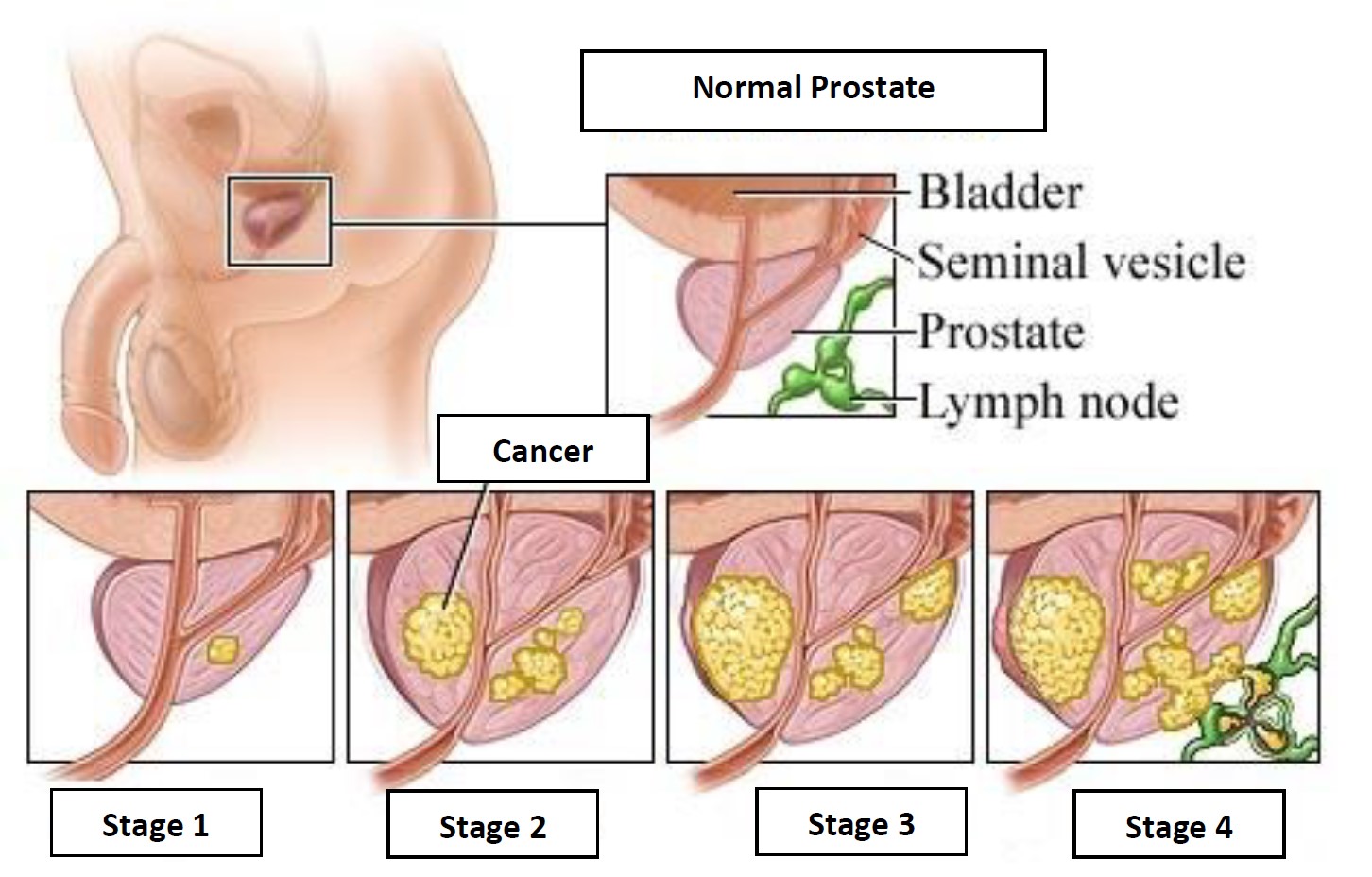
The stages of prostate cancer are classified in 4 stages as in other types of cancer.
Stage 1: Cancer is restricted to the prostate and has spread to a part of the prostate. Gleason score and PSA are very low.
Stage 2: Cancer has progressed more than stage I, but is still restricted to the prostate.
Stage 3: The cancer has spread to the tissue capsule surrounding the prostate. This spread may also involve the semen sac (adjacent to sperm producing glands).
Stage 4: Cancer has spread to lymph nodes and/or organs or semen sac with the structure outside the prostate
Treatment Approaches for Prostate Cancer

The treatment is very closely related to the stage of the diagnosed cancer, we may diagnose prostate cancer in one of these three stages and the treatment is planned by the stage.
The primary treatment methods are as follows:
- Restricted to the prostate, not spreading to surrounding tissues, not spreading to distant organs (Localized prostate cancer): The use of PSA blood test allows us to identify most of the prostate cancer cases at this early stage since our patients are more conscious. The ideal treatment of these patients is the surgery known as "Radical Prostatectomy".
- Spread slightly outside the prostate but does not spread to distant organs: In this patient group, if the patient is below 70 years old, i.e. in the younger group, the operation is the ideal treatment (Radical Prostatectomy), but this surgery alone is usually not enough in this patient group and additional Radiotherapy and sometimes Hormone therapy may be required.
- Metastasized (spread to distant organs) group: Prostate cancers spread to distant organs, especially to the bones and lymph tissues around the large intraabdominal vessels. The primary treatment in the metastasis group is Hormone Therapy. Hormone therapy is administrated by drugs or by surgical excision of both testicles (Bilateral Orchiectomy). Both methods, i.e. drugs or testicular surgery yield the same results. Chemotherapy is another treatment method for this patient group.
- There are also new treatment methods thanks to the developing technology. Mainly: HIFU (high-intensity focused ultrasound wave), focused ultrasound or focal therapy, a treatment method that is applied instead of surgery as a treatment of prostate cancer. In the HIFU treatment, high-intense sound waves are sent to cancer cells in the prostate tissue to destroy cancer cells. i.e. in this method, the cancer focus in the prostate is destroyed by burning. The procedure is performed under general anesthesia when the patient is put into sleep for about 2-3 hours.